Urogenital specimen is required to detect diseases caused by organisms that are transmitted by sexual intercourse and are referred to as venereal diseases.
COMMON PATHOGENS FOUND IN UROGENITAL TRACT:
| URETHRAL SWABS | Neisseria gonorrhoea, Chlamydia trachomatis (serovars D-K) and occasionally Ureaplasma, Mycoplasma and Trichomonas vaginalis. |
| CERVICAL SWABS (from non puerperal women) | Neisseria gonorrhoea, Chlamydia trachomatis (serovars D-K), Streptococcus pyogenes, Herpes simplex virus |
| CERVICAL SWABS (from women with puerperal sepsis or septic abortion) | Streptococcus pyogenes, other beta-haemolytic streptococci, Enterococcus species, anaerobic cocci, Clostridium perfringens, Bacteroides, Proteus, E.coli and other coliforms, Listeria monocytogenes |
| VAGINAL SWABS | Vaginal discharge may be due to infection of the vagina or infection of the cervix or uterus. Pathogens causing vaginal infection include Trichomonas vaginalis, Candida species, and Gardenella vaginalis with anaerobes. |
| GENITAL ULCER SPECIMENS | Treponema pallidum, Haemophilus ducreyi, Calymatobacterium granulomatis, Chlamydia trachomatis (serovars L1, L2, L3), Herpes simplex virus |
NOTES ON PATHOGENS
- The most serious of sexually transmitted disease are syphilis caused by T. pallidum and gonorrhoeae caused by N.gonorrhoeae. U. urealyticum is associated with preterm labour, spontaneous abortion and still birth.
- C. trachomatis and U. urealyticum are associated with non-gonococcal urethritis in men and PID in women. C. trachomatis (Serotypes Ll, L2. L3) cause lymphogranuloma venereum (LGV).
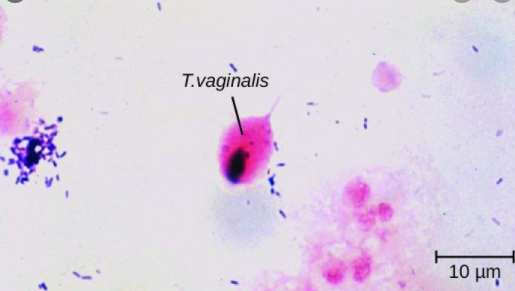
- T. vaginalis (Protozoa) cause acute vaginitis with a purulent & frothy discharge in women.
- C. albicans cause vaginitis producing white discharge.
- G. vaginalis, C. granulomatis also causes genital infection.
- H. duereyi causes chancroid (soft sore).
COLLECTION AND TRANSPORT OF UROGENITAL SPECIMEN:
- Urogenital specimen should be collected by a Medical Officer or an experienced nurse.
- Amies medium is the most efficient medium for transporting urethral, cervical and vaginal swabs. Specimens should be transported in a cool box.
COLLECTION OF URETHRAL DISCHARGE FROM MALE PATIENTS
- Cleanse around the urethral opening using a swab moistened with sterile physiological saline.
- Gently massage the urethra from above downwards. Using a swab, collect a sample of discharge.
- Make a smear of the discharge on a microscope slide by gently rolling the swab on the slide. This will avoid damaging the pus cells which contain the bacteria.
- When culture is indicated, collect a sample of pus on a sterile cotton-wool swab.
- Preferable inoculate a plate of culture media before inserting the swab in a container of Amies transport medium.
- Label the specimens and deliver them to the laboratory as soon as possible.
- Inoculated culture plates must be incubated within 30 minutes.
COLLECTION OF CERVICAL SPECIMENS FROM FEMALE PATIENTS
- A specimen collected from endocervical canal is recommended for isolation of N.gonorrhoeae by culture.
- Use a sterile vaginal speculum to examine cervix and collect specimen.
- Moisten the speculum with sterile warm water, and insert it into the vagina.
- Cleanse the cervix using a swab moistened with sterile physiological saline.
- Pass a sterile cotton-wool swab 20-30 mm into the endocervical canal and gently rotate the swab against the endocervical wall to obtain a specimen.
- When gonorrhoea is suspected, before inserting the swab in Amies transport medium, it is preferable to inoculate a plate of culture medium.
- Label the specimens and deliver to the laboratory as soon as possible. Inoculated culture plates must be incubated within 30 minutes.
COLLECTION OF VAGINAL DISCHARGE TO DETECT T.VAGINALIS, C.ALBICANS AND G.VAGINALIS
- Wet preparation to detect motile T.vaginalis: Use a sterile swab to collect a specimen from the vagina.
- Transfer a sample of the exudate to a microscope slide. Add a drop of physiological saline and mix.
- Cover with a cover glass. Label and deliver to the laboratory for immediate examination.
- Dry smear for gram staining to detect candida and examine for clue cells: Although yeast cells can be seen in a unstained wet preparation, the gram positive cells and pseudohyphae of C.albicans are more easily seen in a gram stained smear.
- Use a sterile swab to collect a specimen from the vagina. Transfer a sample of the exudate to a microscope slide and spread it to make a thin smear.
- Allow the smear to air dry, protected from insects and dust. Label and deliver to the laboratory with the wet preparation.
- Appearance and pH of vaginal discharge in Candida, Trichomonas and Gardenella infections:
- T.vaginalis: Yellow green purulent discharge with pH over 5.
- C.albicans: White odourless discharge with pH below 5.
- G.vaginalis: Grey, offensive, smelling thin discharge with pH over 5. (fishy ammoniacal smell becomes more intense after adding a few drops of 10% potassium hydroxide).
- The normal reaction of vaginal discharge (puberty to menopause) is pH 3.0-3.5.
COLLECTION OF UROGENITAL SPECIMEN TO DETECT T. PALLIDUM
- To detect motile T. pallidum spirochaetes, a specimen must be collected before antibiotic treatment.
- Wearing protective rubber gloves, cleanse around the ulcer (chancre) using a swab moistened with physiological saline.
- Remove any scab which may be present. Caution: T. pallidum spirochaetes are highly infectious.
- Gently squeeze the lesion to obtain serous fluid. Collect a drop on a cover glass and invert it on a microscope slide.
- Immediately deliver the preparation to the laboratory for examination by dark-field microscopy.
COLLECTION OF SPECIMEN TO DETECT C. GRANULOMATIS
- Cleanse around the ulcerated area using a swab moistened with physiological saline.
- Pinch off a small piece of tissue from the edge or base of a lesion. Crush this between two microscope slides.
- Label the slides and deliver them to the laboratory as soon as possible.
- When a delay is anticipated, fix the smears with absolute methanol for 1-2 minutes.
MICROSCOPY FOR VARIOUS CLINICAL CONDITIONS
- Gonorrhoea: Gram stain to detect gram negative diplococci in pus cells in urethral discharge or first voided urine.
- Syphilis: Dark field microscopy to detect motile spirochaetes in serous fluid from genital chancre or skin lesion.
- Trichomoniasis: Fresh wet vaginal preparation to detect motile T.vaginalis
- Candidiasis: Wet vaginal preparation or gram stained smear to demonstrate yeast cells and pseudohyphae.
- G.vaginalis bacterial vaginosis: Gram stained smear of vaginal discharge for epithelial cells with adhering polymorphic bacteria.
- Granuloma inguinale: Giemsa stain of ulcer material to detect intracellular bipolar stained cocco-bacilli.

No comments:
Post a Comment