Preface
Meningitis is an inflammatory condition of the
meninges (membrane surrounding brain and spinal cord) with an infectious
aetiology.
A
typical case of meningitis usually presents with headache, high grade fever,
projectile vomiting, nuchal rigidity and positive Kernig's & Brudzinski’s sign.
Altered mental status, irritability are also common and early presentations in
some cases.
Learning objectives:
1. Different
types of meningitis and their etiologies.
2. Laboratory
methods for analyses of CSF to evaluate a case of meningitis
- Cytology
- Chemical analysis
- Bacteriological analyses by
staining and culture
- Antigen and antibody detection
3. CSF
findings in different types of meningitis
Types of meningitis:
Meningitisis
categorized into three different types depending upon their aetio-pathogenesis
andthe cytology of the Cerebro Spinal Fluid (CSF).
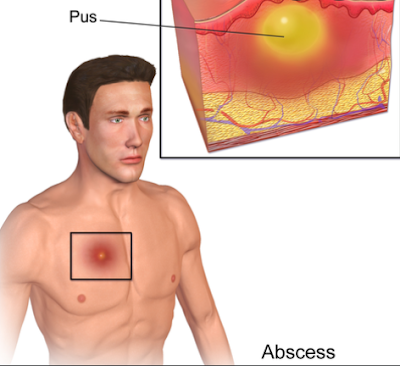
1. Acute
pyogenic meningitis:It is an acute inflammation of the meninges caused mainly
by bacteria. The CSF will typically have large number of pus cells,
predominantly Polymorphs.
2.
Tuberculous meningitis: It is caused by Mycobacterium
tuberculosis. It is one of the most common causes of meningitis in
developing countries. The CSF cytology shows presence of large number of pus cells
with predominant lymphocytes.
3. Aseptic
meningitis: It is caused by viruses, fungi, parasites &some
bacteria. The CSF cytology shows absent or few pus cells with lymphocytic or mixed
cellularity.
Causative agents of meningitis
A) Acute pyogenic meningitis
Bacteria causing meningitis vary according to
the age groups
1. Newborn
(neonatal meningitis):
Group B beta haemolytic Streptococci
(Streptococcus agalactiae): Usually
acquired from vagina while passage of
baby through the birth canal.
Escherichia coli, Klebsiellapneumoniae, other
coliform bacilli: Usually the source of bacteriais the digestive tract.
Pseudomonas
aeruginosa, Listeria monocytogenes etc.
2. Children:
Haemophilusinfluenzae type b (Hib):
Common in young children (2 months to 5 years of age)
Neisseria meningitidis
(Meningococcus)
Streptococcus pneumoniae
(Pneumococcus)
3. Adults:
Neisseria meningitidis
(Meningococcus)
Streptococcus pneumoniae
(Pneumococcus)
Listeria monocytogenes (less common)
4. Hospital
acquired or iatrogenic meningitis:
Various hospital strains i.e. Pseudomonas aeruginosa, Staphylococcus spp.
may be introduced during invasive procedures like lumbar puncture, surgery or
V-P shunts and may lead to meningitis.
B)Tuberculous meningitis: It is
generally secondary to tuberculous lesions elsewhere in the body. It is caused
by Mycobacterium tuberculosis.
C) Aseptic meningitis: It is associated with increased lymphocytes &pleocytosis in CSF with
negative bacterial culture.
1. Viruses: Herpes
simplex viruses (type I more common), Japanese encephalitis virus, Enteroviruses(i.e.
Echo, Coxsackie, Polio) etc.
2. Fungi: Cryptococcus neoformans
3. Parasites:Toxoplasma gondii, Acanthamoeba, Naegleria (may cause
pyogenic meningitis)
4. Bacteria:T.pallidum, Leptospira
5.Meningitis
may be one of the presentations of
certain non-infectious diseases i.e. cancers, connective tissue disorders,
sarcoidosis etc.
Laboratory diagnosis
Sample collection:
1.
The main specimen is CSF, which is analyzed to
confirm clinical diagnosis, to find the type of meningitis and to evaluate
aetiology.
2.
CSF is collected by lumbar puncture with strict aseptic
precautions to prevent iatrogenic infection as wel as contamination of the
specimen.
3.
Sample should be transported immediately to the
laboratory& if possible hand delivered.
4.
If delay in transport of specimen is unavoidable, it should
be kept at 37° C or at room temperature
and should never be kept in refrigerator. If CSF is to be processed only for
viral studies, it can be refrigerated.
5.
Blood sample may be taken for culture examination. The
bacteria causing pyogenic meningitis can usually be isolated from blood
culture.
To increase the isolation rate,
nowadays, it is recommended that the CSF and blood should directly be collected
separately in the bottles of automated culture system (Bactec or BacTAlert ) at
bedside and transported immediately to the laboratory.
Laboratory examination of CSF:
CSF may be processed for,
1.
Cytological study to confirm the diagnosis of meningitis and to evaluate its
type and aetiology:
Total cell
number up to 1-3 / cmm is considered normal in CSF. This will increase in case
of meningitis.
a.
Acute pyogenic meningitis: Total cells
rise up to 1000-10000/
cmm; Predominant cells are neutrophils.
b.
Tuberculosis meningitis: Total cells
rise upto 50-500/cmm;
Predominant cells are lypmhocytes.
c.
Viral meningitis: Total cells rise upto 10-100/cmm;
predominant
cells
are lymphocytes.
2.
Biochemical tests
In
case of meningitis, total protein will increase and sugar will diminish than
normal level.
3.
Microscopic examination for identification of microorganism
CSF is centrifuged and deposits are
examined by following methods
to identify the aetiological
agent
a.
Gram stain: to identify pyogenic bacteria
b.
Z N stain: to detect M.tuberculosis
c.
Negative stain(India ink or nigrosin): to detect Cryptococcus
neoformans
d.
Wet film: to detect parasites like Naegleriafowlerii,
Acanthamoeba,
Toxoplasma gondii
4.
Culture examination for isolation of pathogenic organism
There
are three ways to culture the CSF sample
- A set of culture plates including blood agar, chocolate agar and mac conkey agar are inoculated directly from sample and incubated at 37° C in candle jar (or CO2incubator).
- CSF is centrifuged with precautions to avoid contamination and the deposit is inoculated in a similar set of culture plates.
- 1 - 2 ml of CSF is inoculated in a liquid medium ( i.e. Glucose broth ) or in automated culture system bottle. This will allow growth of even minute number of bacteria if present. When the growth is indicated or observed in liquid medium, it is sub-cultured in similar set of plates to isolate them.
The culture plates are observed for growth after 24-48 hours of incubation. The isolated bacteria are processed for their identification and antibiotic sensitivity testing.
5.
Detection of antigens or antibodies
This is generally done from the supernatant of
the centrifuged CSF sample.
Detection
of antigen:
a.
Capsular polysaccharide of aetiological agent may be
detected by latex agglutination.
The
following capsulated organisms may be detected by this method,
- N.meningitidis(Meningococci),
- Haemophilusinfluenzae,
- Streptococcus pneumoniae(pneumococci)
- Cryptococcus neoformans
b.
Agglutination test may be useful to detect the surface antigens of
-
Group B Streptococci or E.coli which are responsible for
meningitis
in neonates.
Detection
of antibody:
Antibodies
are demonstrable in the following infections, which can be detected by ELISA or
immunofluroscence
- Herpes simplex virus
- Japanese encephalitis
virus
- T. pallidum( neurosyphilis )
Exercise:
An 8 month child presented with fever, neck
rigidity and projectile vomiting and suspected for meningitis.
Q.1 What
are the microscopic findings in case of different kind of meningitis? Which
stains are used to examine the smear prepared from centrifuge of CSF?
Q.2 Which
culture media are used for plating?
Q.3 Which
are the common agents suspected in this case?