Skin and soft tissue infections
Learning
objectives:
Different types
of Skin & soft tissue infections & their aetiological agents
Laboratory
methods to identify the aetiology of various SSTI to guide management
Skin and soft tissue infection (SSTI)
is a comprehensive term which includes all the kinds of infections which
involve skin, muscle and connective tissues. These may be associated with
involvement of deeper parts of body like bones and joints.
Various types of
SSTI and their aetiology
|
Type of infection |
Description |
Aetiological agents |
|
1. Folliculitis |
Infection and inflammation of hair follicle |
Bacteria: Staphylococcus
aureus, Pseudomonas aeruginosa Fungus: Candida albicans,
T.rubrum, Malassezia |
|
2. Furuncles (Boil) |
Skin infection with painful swelling and collection of pus. |
Staphylococcus
aureus |
|
3. Carbuncles |
Individual boils clustered together leading to large infected
mass filled with fluid, pus and dead tissue |
Staphylococcus
aureus |
|
4. Cellulitis |
Diffuse inflammation of connective tissue with involvement of
dermal and subcutaneous layers of skin |
Staphylococcus
aureus & other staphylococci Streptococcus
pyogenes |
|
5. Impetigo |
Highly infectious bacterial skin infection commonly seen in
pre-school children |
Streptococcus
pyogenes Staphylococcus aureus |
|
6. Erysipelas |
Acute infection of skin and superficial lymphatics. Lesions are
typically raised and demarcated. |
Streptococcus
pyogenes |
|
7. Necrotizing infections (Necrotising fascitis) |
Also known as flesh eating disease. It is a rapidly progressing
infection of skin and subcutaneous tissue which can spread across the fascial
plane. |
Streptococcus
pyogenes, Staphylococcus aureus, Clostridium perfringens (
may lead to gas gangrene). Majority times it is a polymicrobial infection. |
|
8. Surgical site infections |
Infection at the site of surgery which occurs within 30 days
after operation. |
Staphylococcus
aureus, Staphylococcus epidermidis, Pseudomonas aeruginosa, members
of enterobacteriaecae family, etc. |
|
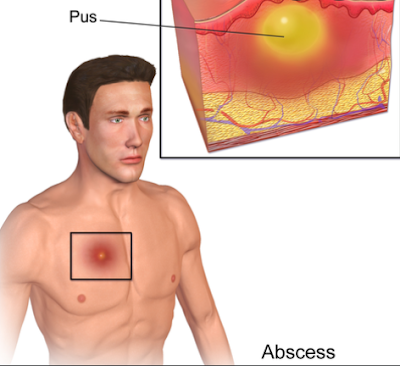
9. Pustule / Abscess |
Collection of pus due to inflammatory processes |
Staphylococcus
aureus is most common. M.tuberculosis is associated with cold abscess. |
|
10. Myositis and pyomyositis |
Infection of muscle with or without pus collection. |
Only myositis in absence of other surrounding site involvement
is more commonly associated with autoimmune disorders rather than directly
due to infection. Pyomyositis is usually caused by Staphylococcus aureus |
|
11. Infection following animal contacts |
|
B. anthracis
(cutaneous anthrax), Bartonella henslae
(Cat scratch disease), E.rhusiopathiae
(Erysipeloid) |
|
12. Infection after animal bite |
|
Mixed aerobic and anaerobic bacteria, Rabies virus |
|
13. Infection after human bite |
|
Mixed aerobic and anaerobic bacteria |
|
14. Mycetoma |
Chronic subcutaneous infection characteristically associated
with multiple sinuses which discharge typical grains |
Eumycetoma: Caused by fungi (e.g. Madurella mycetomatis) Actinomycetoma: Caused by bacteria (e.g. Nocardia sp.) |
|
15. Cutaneous ulcers |
Loss of epidermal & part of dermal tissues. |
B. anthracis,
M. marinum, |
|
16. Burn wounds |
Generally associated with bacteremia |
Pseudomonas
aeruginosa, members of Enterobacteriaceae family. |
|
17. Systemic infections with skin manifestations |
|
a) Petechiae in meningococcaemia. b) Cutaneous ulcers & bullae in V. vulnificus bacteremia. |
|
18. Leprosy |
Systemic disease primarily involving skin, peripheral nerves and
nasal mucosa. |
Mycobacterium leprae |
|
19.
Macule |
Flat, non-palpable discoloration of skin (<5 cm size). If
size exceeds 5 cm, is called as patch |
Dermatophytes
Viral
rashes (e.g. enterovirus, measles) |
|
20.
Papule |
Elevated
lesions usually <5 mm in size that can be felt or palpated |
· Virus: Molluscum contagiosum, Warts (Human Papilloma
virus) · Parasite scabies (Sarcoptes scabiei) |
|
21.
Plaque |
Multiple papules my become confluent to form plaque which are
palpable lesions >5 mm |
|
|
22. Nodule |
Firm lesions >5 cm size |
·
Bacteria Staphylococcus aureus, Mycobacterium marinum · Fungi sporothrix |
|
23. Vesicle |
Fluid-filled lesions with a diameter less than 0.5 cm |
Herpes simplex virus, varicella-zoster virus |
|
24. Bulla |
Fluid-filled lesions with a diameter more than 0.5 cm |
·
Bacteria Clostridium Staphylococcus aureus · Virus Herpes simplex virus |
|
25. Scale |
Excess dead epidermal layer |
Dermatophytes Streptococcus pyogenes |
Laboratory
diagnosis:
Sample
collection:
1.
If there is subcutaneous or deep
pus collection and pus is to be collected through intact skin, It should be
done with sterile syringes and needle. Prior to collection, the surface
area should be cleaned with alcohol. Sample collected in syringe should be
immediately transported to laboratory in it.
2.
If the pus is discharged through
the skin, it should be collected with sterile swab. Prior to collection
of sample, the surface area should always be cleaned with sterile saline (never
use antiseptics). The pus is squeezed and collected with swab.
3.
Skin scrapings or biopsy may be required to collect particularly in dry lesion.
In case of leprosy, skin smear with nasal smear is required or biopsy from
nodular skin lesion and thickened nerves is recommended in some cases.
Laboratory
procedures:
1. Microscopic
examination:
a.
Gram stain: To screen for bacteria
b.
KOH examination: To screen for fungus
c.
Z N stain: For demonstration of M. tuberculosis Atypical mycobacteria. Modified
acid fast stain required for diagnosis
of suspected case of leprosy.
3. Culture
examination:
According
to clinical presentation & type of lesion, the Samples should be cultured
in one or more of following culture media to identify the aetiology of lesion
a.
Simple media: Nutrient agar
b.
Differential media: Mac-Conkey agar
c.
Enriched media: Chocolate agar / Blood agar
d.
Anaerobic media: Robertson's cooked meat broth
e. L J medium: For atypical Mycobacteria
f. Sabouraud's
dextrose agar
Exercise
A 5 year child presented with
multiple painful swellings over the leg and thigh. Pus is discharging from few
lesions.
Q.1 How the samples are collected? (In practical / exam
students should identify the materials used for sample collection and
transportation)
Q.2 Which culture
media are used for isolation of possible aerobic and anaerobic bacterial
pathogen (In practical / exam students may be asked to identify these media and
bacterial growth)
Q.3 Which antibiotics should be tested for its sensitivity against isolated bacteria? (In practical / exam students may be asked for selection of appropriate antibiotic combination circle from the tray; and materials required for sensitivity testing)

No comments:
Post a Comment