Preface
Gastrointestinal
tract teems with a diverse flora. The heterogeneity of commensals makes the
human body all the more prone to infections in diminished states of health
& also poses a tough task for us to label an organism pathogenic or
colonizer or commensal. The chapter here, incorporates an exhaustive list of
microbes from different groups causing diarrheal diseases, which is hoped to
come in handy for the diagnosis.
Commensal
bacterial flora of intestines:
Lactobacilli, Streptococci, Bacteroides, Bifidobacterium,
Peptostreptococcus, Clostridium, Enterobacteriacae. The bacteria
are mostly anaerobes or facultative anaerobes. These commensals provide
competition for nutrition & growth to pathogenic bacteria & thus, do
not easily allow them to thrive.
Learning
objectives:
1. Different
types of diarrheal diseases and their etiologies.
2. How the
stool sample should be transported and analyzed in laboratory?
Following are
the different terminologies used to describe the diarrheal diseases.
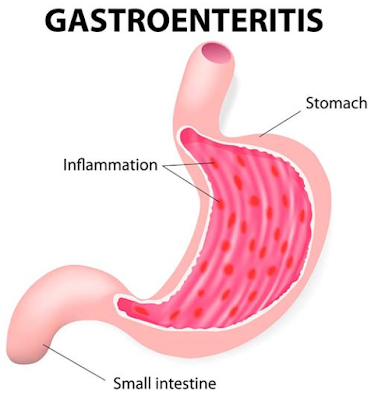
1.
Gastroenteritis: It is defined as the inflammation of mucosa of the gastrointestinal tract (stomach
- "gastro" and intestine - "entero") often
leading to diarrhea, vomiting and abdominal discomfort.
2. Diarrhea: It is
defined as a condition in which loose or liquid stool pass for three or more
times a day. It is the most common presentation of gastroenteritis. Infective
diarrhea is often considered synonymous to gastroenteritis.
3. Dysentery: It is a
condition associated with frequent passage of stool containing mucus, blood or
pus (exudates). It is characteristically associated with abdominal cramps,
tenesmus and fever.
4. Food
poisoning: It is a condition of acute gastroenteritis originating
due to consumption of food containing large number of bacteria or their
products like toxins; which after entry in gastrointestinal tract, without
undergoing further multiplication or toxin production immediately and with very
short incubation period lead to pathogenesis and clinical manifestations.
5. Colitis: Inflammatory
condition of large bowel (colon) is called colitis. Many organisms may cause
only colitis or enterocolitis leading to watery diarrhea or dysentery.
Patients of
infectious diarrhea have two kinds of presentations:
1. Watery diarrhea
2. Dysentery
Causative
agents of watery diarrhea
A. Bacteria:
Vibrio cholerae (rice watery diarrhea)
Entero-Pathogenic
Escherichia coli (paediatric
diarrhea)
Entero-Toxigenic
Escherichia coli (traveler's
diarrhea/Montezuma’s revenge/ Delhi belly )
Campylobacter spp.
Salmonella sp. (S.typhimurium,
S.enteritidis etc)
Clostridium difficile (antibiotic associated colitis)
B. Viruses:
Rotavirus
(most common cause of paediatric diarrhea)
Norwalk virus
Calici virus
Astrovirus
Adenovirus
C. Parasites
Giardia intestinalis ( usually leads to fatty diarrhea )
Cryptosporidium parvum (Paediatric diarrhea or diarrhea in immuno
compromised patients)
Isospora belli (diarrhea in immuno compromised patients)
Helminths: Hymenolepsis nana, Trichuris trichiura,
Strongyloides stercoralis, Ascaris lumbricoides, Ancyclostoma duodenale etc.
D. Fungus: Candida albicans
E. Bacteria
associated with food poisoning
Bacterial food poisoning are of two
types
1. Toxic type: Bacterial
toxins lead to gastroenteritis
Staphylococcus aureus (Common with milk and milk products)
Bacillus cereus (Common with fried rice)
Clostridium perfringens
Clostridium botulinum (Common with canned food)
2. Infective type: Direct
bacteria invade mucosa and cause gastroenteritis
Vibrio parahaemolyticus
Campylobacter
jejuni
Yersinia
enterocolitica
Salmonella
typhimurium
Causative
agents of dysentery:
According to
the aetiological agents, dysentery is divided in two types
A. Bacillary
dysentery: caused by bacteria
Shigella
spp.
Entero-Invasive Escherichia coli
Entero-haemorrhagic Escherichia coli
B. Amoebic
dysentery: Caused by Entamoeba
histolytica
Laboratory
diagnosis
A. Stool
analysis:
Sample
collection:
Stool is the
most informative sample to evaluate aetio-pathogenesis of diarrheal diseases.
In paediatric patients or critically debilitated patients with severe watery
diarrhea, if it is not possible to collect sample, rectal swab may be taken.
Intestinal aspiration with help of endoscope may be taken to diagnose certain
parasitic infection (e.g. hook worm present in small intestine, E.histolytica present in the ulcers of
large intestine).
Sample
transport:
Sample as it is should be
immediately transported to laboratory.
If there is delay in transport,
according to suspected bacterial pathogens. it should be transported in
following transport media,
1. In suspected cases of Cholera:
Venkatraman -
Ramakrishnan (VR) medium
Cary-Blair medium
Alkaline peptone water (if
sample is transported within a day )
2. In suspected cases of
infection by enterobacteriacae members:
Glycerol buffered saline
3.
In suspected viral infections:
The
sample should be refrigerated if not processed within 2 hours. Rectal swabs may
be stored & transported in Modified Stuart’s medium or Viral Transport
Medium.
Sample
processing:
1. Gross
examination: Direct appearance may help to evaluate infective
aetiology
- Rice watery stool is most commonly
seen in Vibrio cholerae
- Presence of gross blood or pus is
indicative of dysentery
- Foul smell suggestive of fatty
diarrhea is a common presentation of giardiasis
- Helminths like round worm, hook
worm, thread worm, tape worm, whip worm may be grossly visible in the stool.
2.
Microscopic examination:
Stool should be examined
microscopically for following findings
1.
Pus cells: Presence of pus cells is suggestive of invasive infection with
marked inflammation
2. RBCs: Presence of RBCs is
suggestive of dysentery
3. Parasites: On microscopic
examination, following parasites may be seen in stool,
Cysts or/and trophozoites of Entamoeba histolytica, Giardia intestinalis.
Oocysts of Cryptosporidium parvum, Isospora belli.
Ova of H. nana, hook worm, round worm, whip worm, tape worm and thread
worm. Larvae of S.stercoralis.
4.
Fungus: Yeast cells - Candida may be
demonstrated. Its significance should be evaluated with other clinical
background; generally if pseudohyphae is seen along with budding yeast cells,
it is considered significant.
5. Bacteria: A large number of
bacteria are normally present in stool. It is not possible to differentiate
normal bacteria from pathogenic bacteria by microscopic examination. However, presence of Vibrio cholerae may be
indicated by demonstration of its specific darting type of motility with
hanging drop preparation.
6.
Other structures: i.e. Charcot-Leyden (CL) crystals are present in amoebic
dysentery.
3. Culture
examination:
Stool specimen normally contains
large number of commensals. These bacteria may affect selective isolation of
pathogenic bacteria. Escherichia coli,
a common cause of diarrhea is also a
common commensal of normal stool. So, for culture examination of stool, we need
different sets of culture media containing enrichment and selective media along
with simple and differential media according to suspected aetiological agents.
Culture media
used:
1. Simple
media: Nutrient agar
2.
Differential media: Mac conkey agar
3. Enrichment
media: Selenite F broth or
tetrathionate broth: For Salmonella and Shigella
Alkaline
peptone water: For Vibrio cholerae
4. Selective
media: TCBS: For Vibrio cholerae
Wilson-Blair
medium: For Salmonella
DCA or XLD
agar: For Shigella and Salmonella
Isolated
bacteria are identified and processed for antibiotic sensitivity testing.
Typing of bacteria may be needed for epidemiological purpose.
4. Antigen
Detection :
E. coli O157:H7 -
Enzyme linked Immuno Assays (EIAs).
Rotavirus -
Enzyme linked Immuno Assays &
Latex Agglutination Tests (LATs).
C. difficile -
Toxin A and/ toxin B detection.
B. Analysis
of other specimens:
Rectal swab: In
paediatric patients with severe watery diarrhea, if it is not possible to collect
stool sample, rectal swab may
be taken and processed for culture examination.
Intestinal aspiration
with help of endoscope may be taken to diagnose certain parasitic infection
(e.g. hook worm present in small intestine)
Intestinal biopsy: May
be taken by endoscopy which may show pathogenic organism on histopathological
examination. e.g. E.histolytica present in ulcer of large intestine, H.pylori present in gastric biopsy.
Vomited material:
Particularly useful in case of food poisoning for detection of bacterial toxins
Food sample: Should be
taken to find out agent responsible for food poisoning.
Exercise:
A 20 year old
male patient presented with acute abdominal pain and diarrhoea. Microscopic
examination of stool is suggestive of dysentry. Stool sample is required to
evaluate for aetiology at the microbiology laboratory situated at distant
place.
Q.1 Which culture media are required for
transport of speciemen?
Q.2 For recovery of possible pathogen which
culture media should be employed?
Q.3 Which are the suspected bacteria?
Q.4 Enlist the Bio-chemical test used for
differential identification of enterobacteriacae member.
& also poses a tough task for us to label an organism pathogenic or
colonizer or commensal. The chapter here, incorporates an exhaustive list of
microbes from different groups causing diarrheal diseases, which is hoped to
come in handy for the diagnosis.
Commensal
bacterial flora of intestines:
Lactobacilli, Streptococci, Bacteroides, Bifidobacterium,
Peptostreptococcus, Clostridium, Enterobacteriacae. The bacteria
are mostly anaerobes or facultative anaerobes. These commensals provide
competition for nutrition & growth to pathogenic bacteria & thus, do
not easily allow them to thrive.
Learning
objectives:
1. Different
types of diarrheal diseases and their etiologies.
2. How the
stool sample should be transported and analyzed in laboratory?
Following are
the different terminologies used to describe the diarrheal diseases.
1.
Gastroenteritis: It is defined as the inflammation of mucosa of the gastrointestinal tract (stomach
- "gastro" and intestine - "entero") often
leading to diarrhea, vomiting and abdominal discomfort.
2. Diarrhea: It is
defined as a condition in which loose or liquid stool pass for three or more
times a day. It is the most common presentation of gastroenteritis. Infective
diarrhea is often considered synonymous to gastroenteritis.
3. Dysentery: It is a
condition associated with frequent passage of stool containing mucus, blood or
pus (exudates). It is characteristically associated with abdominal cramps,
tenesmus and fever.
4. Food
poisoning: It is a condition of acute gastroenteritis originating
due to consumption of food containing large number of bacteria or their
products like toxins; which after entry in gastrointestinal tract, without
undergoing further multiplication or toxin production immediately and with very
short incubation period lead to pathogenesis and clinical manifestations.
5. Colitis: Inflammatory
condition of large bowel (colon) is called colitis. Many organisms may cause
only colitis or enterocolitis leading to watery diarrhea or dysentery.
Patients of
infectious diarrhea have two kinds of presentations:
1. Watery diarrhea
2. Dysentery
Causative
agents of watery diarrhea
A. Bacteria:
Vibrio cholerae (rice watery diarrhea)
Entero-Pathogenic
Escherichia coli (paediatric
diarrhea)
Entero-Toxigenic
Escherichia coli (traveler's
diarrhea/Montezuma’s revenge/ Delhi belly )
Campylobacter spp.
Salmonella sp. (S.typhimurium,
S.enteritidis etc)
Clostridium difficile (antibiotic associated colitis)
B. Viruses:
Rotavirus
(most common cause of paediatric diarrhea)
Norwalk virus
Calici virus
Astrovirus
Adenovirus
C. Parasites
Giardia intestinalis ( usually leads to fatty diarrhea )
Cryptosporidium parvum (Paediatric diarrhea or diarrhea in immuno
compromised patients)
Isospora belli (diarrhea in immuno compromised patients)
Helminths: Hymenolepsis nana, Trichuris trichiura,
Strongyloides stercoralis, Ascaris lumbricoides, Ancyclostoma duodenale etc.
D. Fungus: Candida albicans
E. Bacteria
associated with food poisoning
Bacterial food poisoning are of two
types
1. Toxic type: Bacterial
toxins lead to gastroenteritis
Staphylococcus aureus (Common with milk and milk products)
Bacillus cereus (Common with fried rice)
Clostridium perfringens
Clostridium botulinum (Common with canned food)
2. Infective type: Direct
bacteria invade mucosa and cause gastroenteritis
Vibrio parahaemolyticus
Campylobacter
jejuni
Yersinia
enterocolitica
Salmonella
typhimurium
Causative
agents of dysentery:
According to
the aetiological agents, dysentery is divided in two types
A. Bacillary
dysentery: caused by bacteria
Shigella
spp.
Entero-Invasive Escherichia coli
Entero-haemorrhagic Escherichia coli
B. Amoebic
dysentery: Caused by Entamoeba
histolytica
Laboratory
diagnosis
A. Stool
analysis:
Sample
collection:
Stool is the
most informative sample to evaluate aetio-pathogenesis of diarrheal diseases.
In paediatric patients or critically debilitated patients with severe watery
diarrhea, if it is not possible to collect sample, rectal swab may be taken.
Intestinal aspiration with help of endoscope may be taken to diagnose certain
parasitic infection (e.g. hook worm present in small intestine, E.histolytica present in the ulcers of
large intestine).
Sample
transport:
Sample as it is should be
immediately transported to laboratory.
If there is delay in transport,
according to suspected bacterial pathogens. it should be transported in
following transport media,
1. In suspected cases of Cholera:
Venkatraman -
Ramakrishnan (VR) medium
Cary-Blair medium
Alkaline peptone water (if
sample is transported within a day )
2. In suspected cases of
infection by enterobacteriacae members:
Glycerol buffered saline
3.
In suspected viral infections:
The
sample should be refrigerated if not processed within 2 hours. Rectal swabs may
be stored & transported in Modified Stuart’s medium or Viral Transport
Medium.
Sample
processing:
1. Gross
examination: Direct appearance may help to evaluate infective
aetiology
- Rice watery stool is most commonly
seen in Vibrio cholerae
- Presence of gross blood or pus is
indicative of dysentery
- Foul smell suggestive of fatty
diarrhea is a common presentation of giardiasis
- Helminths like round worm, hook
worm, thread worm, tape worm, whip worm may be grossly visible in the stool.
2.
Microscopic examination:
Stool should be examined
microscopically for following findings
1.
Pus cells: Presence of pus cells is suggestive of invasive infection with
marked inflammation
2. RBCs: Presence of RBCs is
suggestive of dysentery
3. Parasites: On microscopic
examination, following parasites may be seen in stool,
Cysts or/and trophozoites of Entamoeba histolytica, Giardia intestinalis.
Oocysts of Cryptosporidium parvum, Isospora belli.
Ova of H. nana, hook worm, round worm, whip worm, tape worm and thread
worm. Larvae of S.stercoralis.
4.
Fungus: Yeast cells - Candida may be
demonstrated. Its significance should be evaluated with other clinical
background; generally if pseudohyphae is seen along with budding yeast cells,
it is considered significant.
5. Bacteria: A large number of
bacteria are normally present in stool. It is not possible to differentiate
normal bacteria from pathogenic bacteria by microscopic examination. However, presence of Vibrio cholerae may be
indicated by demonstration of its specific darting type of motility with
hanging drop preparation.
6.
Other structures: i.e. Charcot-Leyden (CL) crystals are present in amoebic
dysentery.
3. Culture
examination:
Stool specimen normally contains
large number of commensals. These bacteria may affect selective isolation of
pathogenic bacteria. Escherichia coli,
a common cause of diarrhea is also a
common commensal of normal stool. So, for culture examination of stool, we need
different sets of culture media containing enrichment and selective media along
with simple and differential media according to suspected aetiological agents.
Culture media
used:
1. Simple
media: Nutrient agar
2.
Differential media: Mac conkey agar
3. Enrichment
media: Selenite F broth or
tetrathionate broth: For Salmonella and Shigella
Alkaline
peptone water: For Vibrio cholerae
4. Selective
media: TCBS: For Vibrio cholerae
Wilson-Blair
medium: For Salmonella
DCA or XLD
agar: For Shigella and Salmonella
Isolated
bacteria are identified and processed for antibiotic sensitivity testing.
Typing of bacteria may be needed for epidemiological purpose.
4. Antigen
Detection :
E. coli O157:H7 -
Enzyme linked Immuno Assays (EIAs).
Rotavirus -
Enzyme linked Immuno Assays &
Latex Agglutination Tests (LATs).
C. difficile -
Toxin A and/ toxin B detection.
B. Analysis
of other specimens:
Rectal swab: In
paediatric patients with severe watery diarrhea, if it is not possible to collect
stool sample, rectal swab may
be taken and processed for culture examination.
Intestinal aspiration
with help of endoscope may be taken to diagnose certain parasitic infection
(e.g. hook worm present in small intestine)
Intestinal biopsy: May
be taken by endoscopy which may show pathogenic organism on histopathological
examination. e.g. E.histolytica present in ulcer of large intestine, H.pylori present in gastric biopsy.
Vomited material:
Particularly useful in case of food poisoning for detection of bacterial toxins
Food sample: Should be taken to find out agent responsible for food poisoning.