Step 1: The diagnosis of a microbial infection begins with an assessment of clinical and epidemiologic features, leading to the formulation of a diagnostic hypothesis.
Step
2: Anatomic localization of the infection with
the aid of physical and radiologic findings (e g right lower lobe pneumonia,
sub-phrenic abscess) is usually included for clinical diagnosis of infectious diseases.
However
in some instances, site of infection can’t be localized; then, a multi tasking
approach will be required.
Step
3: Having clinical diagnosis based upon above
two steps will help to predict a possible
etiologic agent or a number of possible etiologic agents based on
knowledge of infectious syndromes and their courses.
The
specific cause is then established by the application of methods described in next
chapters.
A
combination of science and art on the part of both the clinician and microbiologist
is required
Step
4: The clinician must select the appropriate tests and specimens to be processed and,
where appropriate, suggest the suspected etiologic agents to the laboratory.
Step
5: The microbiologist must use the methods that will demonstrate the probable agents & provide
evidence of existence of causative etiological agent, and be prepared to
explore other possibilities suggested by the clinical situation or by the
findings of the laboratory examinations.
Most
important: The best results are obtained when
communication between the clinician and microbiologist is maximal.
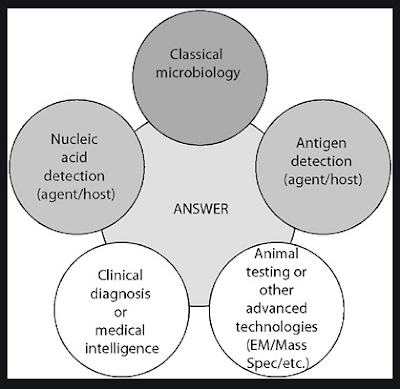
The
general approaches to laboratory diagnosis vary with different microorganisms
and infectious diseases. However, the types of methods are usually some
combination of
(A) The investigations which supports clinical diagnosis of
possibilities of infection:
e.g. Total & Differential count of WBCs,
Stool / Urine routine & microscopic examination etc.
(B) The investigations which gives direct evidence of
presence of aetiological organisms in the specimen:
These includes,
1. Direct Microscopic examination: Gram stain, Z N stain,
KOH examination for fungus etc
2. Culture techniques: For isolation & confirmative
identification of aetiological agent. This also helps to perform antimicrobial
sensitivity testing of the pathogen, which in turn helps to select treatment
for patient.
3. Antigen detection: By immunological techniques e.g.
Immuno-chromatography
4. Nucleic Acid Detection: By various Nucleic Acid
Amplification Techniques (NAAT) e.g. Polymerase Chain Reaction (PCR)
(C) The investigations which indirectly suggest possibility
of infection with particular organisms
This includes various immunological tests those
indicate immune response of the body against particular pathogens
1. Detection of antibodies in patient’s serum against
specific pathogen
2. Detection of cell mediated immune response in patient
against specific pathogen by in vivo (Skin test) or in vitro methods
- All diagnostic approaches begin with some kind of
specimen collected from the patient.
- The primary
connection between the clinical encounter and the diagnostic laboratory is the
specimen submitted for processing. If it is not appropriately chosen and/or
collected, no degree of laboratory skill can rectify the error. Failure at the level of specimen collection
is the most common reason for failing to establish an etiologic diagnosis,
or worse, for suggesting a wrong diagnosis.
-
In the case
of bacterial infections, the primary problem lies in distinguishing resident or
contaminating normal floral organisms from those causing the infection.

No comments:
Post a Comment