Learning
objectives:
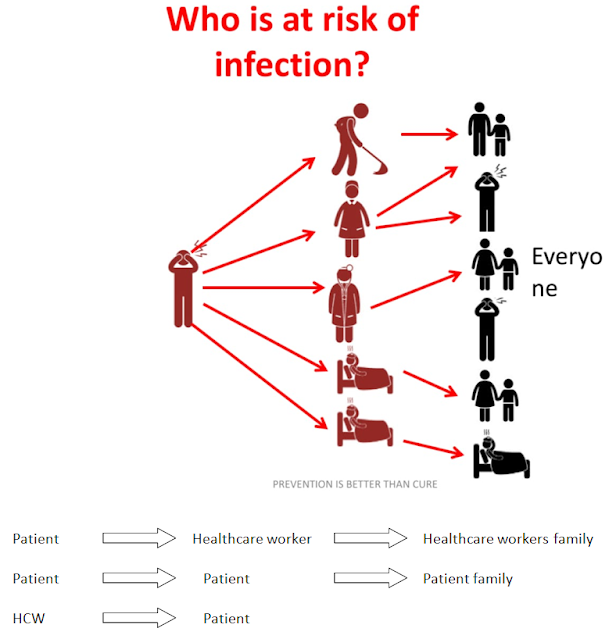
Infection Control
Precautions: Used to reduce transmission of
microorganisms in Hospital & laboratory
Infection control precautions includes
1.
Standard precautions
a.
hand hygiene &
b.
personal protective equipment (PPE)
2.
Transmission based precautions
Standard
Precautions:
·
Standard Precautions are the minimum infection prevention practices that
apply to, all patient care regardless of suspected or confirmed infection
status of the patient, in any setting where health care is delivered.
·
They are the set
of work practices used to minimize transmission of HAI (health care associated
infection) s.
·
They include measures
to be used when providing care to/handling –All individuals, all specimens
(blood or body fluids),
all needles and sharps.
·
Standard
precaution = Universal precautions +
Contact transmission(skin/mucosal) prevention
Objectives
of Standard Precautions
There are two objectives
- The first is to prevent cross infection.
- The second objective is to protect HCW from blood borne as well as other contagious infection.
Components of standard precautions
1. Universal precautions
2. Hand hygiene
3. Personal protective equipment
4. Spillage cleaning
5. Respiratory hygiene and cough etiquette
6. Transmission-based precautions:
7. Biomedical waste including sharp handling
8. Disinfection
Universal
precautions
Blood, blood products, all body fluids, and materials
contaminated with them areconsidered as infectious for HIV, HBV, HCV, and other
blood borne pathogens. Universal precautions includes use of appropriate
precautions to prevent exposure to skin and mucous membranes.
·
Wear gloves, gowns/aprons, masks, and goggles, while
handling all potentially infectious material.
·
Take special care of handling sharp objects (like
needles, lancets, scalpels, etc.) to avoidinjuries:
o
Avoid unnecessary use of sharps and needles
o
Disposable needles should be used
o
Handle hollow bore needles with care as it may lead to
deep injuries
o
Never recap needles
o
Never break/bend needles by hand
o
Needles/sharps should not be left on trolleys and bed
side tables and must be disposedof immediately
o
Never pass used sharps from one person to another
directly
- ·
Dispose sharps in a puncture resistant container
containing 1% sodium hypochlorite solution.
- ·
Thoroughly wash hands with water and soap after
removing gloves, after handling infectious materials, before leaving the
laboratory area, and immediately after any contamination of skin surfaces.
- ·
Work surfaces should be decontaminated with 0.1 %
sodium hypochlorite solution.
- ·
Laboratory personnel should refrain from mouth pipetting,
eating, drinking, or smoking inthe work area.
- ·
Access to the laboratory should be limited to trained
personnel only.
- ·
Food and drink must be stored in refrigerators in
areas other than the work area.
- · All HCPs must be immunized against HBV.
Hand hygiene
Hands
are the main source of transmission of infections during healthcare.Hand
hygiene is therefore the most important measure to avoid the transmission of
harmful microbes and prevent healthcare-associated infections.
·
Hand
hygiene is a general term that applies to either handwashing, antiseptic hand
wash, antiseptic hand rub, or surgical hand antisepsis.
·
Indications for hand
hygiene:
2. After barehanded touching of instruments, equipment, materials, and other objects likely to be contaminated by blood, saliva, or respiratory secretions.
3. Before and after treating each patient.
4. Before putting on gloves and again immediately after removing gloves.
5. Gloves are not a substitute for hand washing.
Personal
Protective Equipments (PPE)
Used to protect the skin and mucous membranes of Health Care Worker(HCW)s from exposure to blood and/or body fluids; & from the HCW’s hands to the patient during sterile and invasive procedures.
Spillage
management:
Blood
spillage may occur because a laboratory sample breaks or because there is
excessive bleeding during phlebotomy. In this situation, clean up the spillage
and record the incident, using the following procedure.
- Evacuate the contaminated area
- Wear a pair of non-sterile gloves preferably heavy duty ones
- Mark the contaminated area with a chalk or pen
- Use a pair of forceps or tongs or a pan and brush to sweep up as much of the broken glass (or container) as possible. Do not pick up pieces with your hands (even with gloves)
- Discard the broken glass in a sharps container. If this is not possible due to the size of the broken glass, wrap the glass or container in several layers of paper and discard it carefully in a separate container. Do not place it in the regular waste container
- Use disposable paper towels / absorbent material (gauze pieces, cotton, blotting paper, etc.) to absorb as much of the sample as possible
- Saturate the area again with 1% sodium hypochlorite (which should be prepared daily) from the periphery to the centre. Wait for 15-20 minutes
- Discard the absorbent material and wipe the area clean with a disinfectant
- Clean and disinfect the forceps/tongs/ brush and pan
- Remove gloves and discard them
- Wash hands carefully with soap and water and dry thoroughly with single-use towels
- Record the incident in the incident book if a sample was lost, or persons were exposed to blood and body fluids
Respiratory hygiene and cough etiquette
- Should be followed by anyone with signs and symptoms of a respiratory infection, regardless of the cause.
- Cover the nose/mouth with single-use tissue paper when coughing, sneezing, wiping and blowing noses
- If no tissues are available, cough or sneeze into the inner elbow rather than the hand
- Follow hand hygiene after contact with respiratory secretions and contaminated objects/materials
- Keep contaminated hands away from the mucous membranes of the eyes and nose
- In high-risk areas of airborne transmission such as pulmonary medicine OPD: Give mask to the patients with cough and make separate queue away from the general queue
- Sputum collection should be done in an open space or in a well- ventilated room\
Transmission-based precautions:
Standard
precautions are used for all patients regardless of their diagnoses to ensure
protection of the health care worker and the patient. For certain highly transmissible or
epidemiologically important pathogens, transmission-based precautions are used
in addition to standard precautions:
a) Contact
precautions:
-
For protection against skin-to-skin contact and physical transfer of
microorganisms to a host from a source e.g. :Discharging wounds are common
source of Methicillin Resistant Staphylococcus Aureus (MRSA)
-
Precautions: Isolation, hand washing,
use of gloves
b) Precaution
from droplet infections
- For infectious agents with droplet nuclei > 5 microns, through cough or sneezing e.g., Pertussis, Influenza, Meningococcal meningitis
- Precautions: -isolation room, use of surgical mask
c) Precautions
from airborne transmission
- For infectious agents with droplet nuclei < 5 microns e.g., Tuberculosis, Measles, Chickenpox
- Precautions: -Isolation rooms with negative pressure, Air cycling >12/hour, HEPA filters
-Use respirators or N95 mask, patient will use a surgical mask
d) Reverse isolation
-
barrier protection to protect patients that are highly susceptible to
infection.



No comments:
Post a Comment