Respiratory tract infection is one of the
commonest infections seen in the community. Upper respiratory tract infection
(URTI) specifically is noted to occur round the year through the seasonal
changes, mostly with viral etiology. Infections of respiratory tract can have
different types of presentations. Mainly, they are divided into Upper
respiratory tract infections (URTI) & Lower respiratory tract infections
(LRTI) based on the part of the respiratory system affected. Any respiratory
infection above the level of glottis or vocal cord is URTI & below it is
LRTI.
Learning objectives
· Different
infectious conditions of respiratory tract & their etiologies
· Sample
collection for evaluation of RTI - Sputum; lavage/swabs/aspiration from
relevant sites etc.
· Staining methods and culture technique for sample analyses.
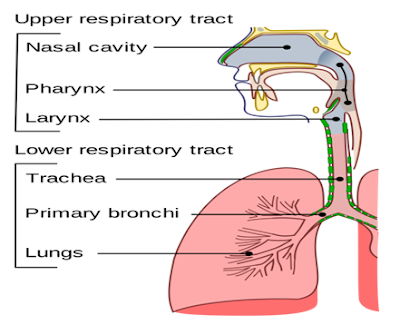
Anatomy:
Part of respiratory tract above
the glottis or vocal cord is called upper respiratory tract. The major passages
and structures of the upper respiratory tract include the nose or nostrils,
nasal cavity, mouth, throat (pharynx), and voice box (larynx). Upper
respiratory tract provides innate protection from development of lower
respiratory tract infections through (1) Filtration action of nasal hair, (2) Mucus
secretion by mucosa which traps small particles, (3) Rich blood supply to nasal
epithelium which warms and moisten the inhaled air, (4) Lymphatic tissue like
tonsils and adenoids present in pharynx those protect against infection by
releasing T & B lymphocytes & (5) Epiglottis of larynx that prevents
food and liquid to enter in to lower respiratory tract.
Types of upper respiratory tract infection
1.
Local inflammation: i.e. Sore throat
(Tonsilitis or Pharyngitis), Rhinitis, Epiglottitis, Sinusitis, Otitis media
etc.
2.
Abscess formation: Faucial or Tonsilar
3.
Ulcer formation: mouth, throat etc.
4.
Diphtheria
5.
Pertussis
6.
Quinsy (Infection of retropharyngeal
space)
1.
Causative agents
of Upper respiratory Tract Infections
Rhinitis
Mostly
caused by virus
·
Rhinovirus
·
Influenza virus
·
Parainfluenza virus
·
Respiratory syncitial virus
·
Coronavirus
·
Adenovirus
· Human
metapneumovirus
Sinusitis
1.
Acute
Bacteria
·
Streptococcus pneumoniae
·
Haemophilus influenzae
·
Moraxella catarrhalis
· Pseudomonas
species and other gram negative bacilli that can cause
nosocomial sinusitis
Virus
·
Rhinoviruses
·
Influenza viruses
·
Parainfluenza viruses
2.
Chronic sinusitis
·
Obligate anaerobes
·
Staphylococcus aureus
·
Fungus like Aspergillus, Mucor
Pharyngitis
and tonsillitis
Bacteria
·
Streptococcus pyogenes
·
Corynebacterium diphtheriae
·
Mycoplasma pneumoniae
· Vincent
angina: Treponema vincentii
Virus
·
Influenza viruses
·
Parainfluenza viruses
·
Coxsackie virus A
·
Rhinoviruses
·
Coronavirus
·
Epstein-Barr virus
·
Adenoviruses
Fugal
·
Candida albicans
Laryngitis
Mostly
viral agent
·
Influenza viruses
·
Parainfluenza viruses
·
Adenovirus
·
Coronavirus
·
Human metapneumovirus
Exudative
tonsillitis / Membrane or exudates present
·
Corynebacterium diphtheria
·
Streptococcus pyogenes
·
Ebstein-Barr virus
Epiglottis
· Most
common agent Haemophilus influenzae type B
Laryngo
tracheobronchitis (Croup)
·
Parainfluenza virus
·
Influenza virus
·
Rspiratory syncytial virus
·
Adenovirus
2.
Clinical
presentation:
Rhinitis
· Running
nose
Sinusitis
· Headache
· Thick
nasal mucus
· Plugged
nose
Pharyngitis
and tonsillitis
· Sore
throat
· Difficulty
in swallowing
Laryngitis
· Hoarseness
of voice
· Lowering
and deepening of voice
Epiglottis
· Fever
· Difficulty
in swallowing
· Inspiratory
stridor
Laryngo
tracheal bronchitis
· Hoarseness
of voice
· Fever
· Cough
(Harsh or barking non productive cough)
· Inspiratory
stridor
3.
Laboratory
diagnosis of Upper respiratory tract infection
Specimen
collection:
· Nasal
/ throat swab: two throat swab samples should be collected from affected part,
one for direct examination and one for culture.
· Part
of membrane & swab from fragile margin of membrane
· Nasopharyngeal
swab or aspirate for viral diagnosis
Processing
the specimen
Microscopy
Gram
stain:
Bacteria
can be identified based on their morphology and shape.
Interpretation:
Bacteria demonstrated in gram stain examination should be carefully
interpretated i.e. presence of gram positive cocci in chains suggestive of
Streptococcus species which may be commensals (streptococcus viridians) or
pathogenic (streptococcus pyogenes).
Albert
stain:
To
demonstrate the Corynebacterium diphtheriae
Interpretation:
presence of bluish-black metachromatic granules either at one end or both ends
and cuneiform arrangement (Chinese letter pattern arrangement) of bacilli
suggestive of C.diphtheriae
Immunofuorescence
microscopy:
To
demonstrate presence of antigens of viruses causing URTI
Culture:
For
bacteriological culture specimen should be inoculated onto following culture
media
· Blood
agar
· Chocolate
agar
· MacConkey’s
agar
· Loeffler’s
serum slope and potassium tellurite blood agar (for isolation of Corynebacterium
diphtheria in suspected cases of Diphtheria).
· Sabouraud
dextrose agar (SDA) is used if fungal infection is suspected.
Interpretation:
-
Bacterial growth can be identified by
colony morphology / pigment production / haemolysis on blood agar & / or
colour of colony on Mac Conkey agar.
-
On Loeffler’s serum slope media C.diphtheriae
produces small, circular glistening, white with yellowish tinged colonies
within 6-8 hours while on potassium tellurite blood agar C.diphtheriae
produces black colonies due to reduction of tellurite to tellurium after 48
hours. Tellurite blood agar commonly helps in isolation of C.diphtheriae
from carrier.
-
On SDA: Candida species produces smooth,
creamy, white, pasty colonies. Aspergillus / mucor produce growth of mycelium.
Molecular
test
-
Polymerase chain reaction method is
used for diagnosis of various virus infections i.e. Swine flu / bird flu
-
Multiplex PCR assay are available
where multiple primers targeting the genes specific for each of the suspected
agents of URTI are used.
Exercise:
Case
study:
A
5-year old child with history of fever and throat pain for 3 days was brought
to ENT OPD. On examination, he was febrile (101˚F) and throat
examination revealed pustules over tonsils. His throat swab was sent to the
microbiology laboratory and was subjected to culture and sensitivity testing.
1.
What is your clinical diagnosis?
2.
What are etiological agents,
pathogenesis and clinical features of this condition?
3.
Discuss your approach for laboratory
diagnosis?

No comments:
Post a Comment