 |
Tuberculosis is one of the most common infectious diseases in the world. Almost one third of the world's population is thought to have been infected with Mycobacterium tuberculosis, with new infection occurring at a rate of about one per second.
Tuberculosis in
human beings is usually caused by
M. tuberculosis and rarely by M. bovis. Mycobacteria other than tuberculosis (MOTT)
may also account for up to 10% of all mycobacterial infections.
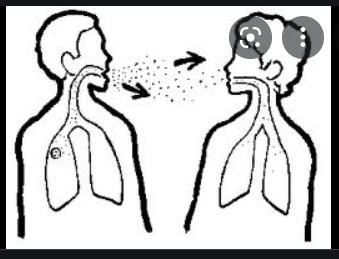
Pulmonary tuberculosis is the most
common clinical presentation, however it may affect many other parts of body. A
majority of these infections spread through inhalation of airborne droplet
nuclei containing bacteria. Many a times infection remains latent and may be
cured without any clinical presentation, leaving the patient hypersensitive to the
bacteria, with T cell mediated immunity. In clinically active tuberculosis,
classical symptoms are chronic cough with blood tinged sputum, low grade fever,
night sweats and weight loss.
Extra-pulmonary
tuberculosis is also not uncommon. It may manifest as tuberculous meningitis, lymph-adenopathy, renal
tuberculosis, osteo-articular tuberculosis etc. Tuberculosis involving
lymphnode and bone may be associated with collection of pus and abscess
formation. Such abscesses are known as cold abscesses.
Learning objectives:
Whenever a patient is to be evaluated for infection
at microbiology laboratory, the collected speciemen must be screened for
possibility of tuberculous infection by simple techniques i.e. Z N stain,
cytology, histopathology, ESR etc.
Whenever a patient is suspected for having
tuberculosis, for laboratory diagnosis students must know
1.
The different modalities are available for laboratory diagnosis of tuberculosis
A.
Microscopic methods: Z. N stain, Auramin phenol stain
B.
Culture methods: Conventional and automated methods
C.
Identification of mycobacterial isolate: Biochemical reaction
D.
Anti tuberculous drug sensitivity
E.
Nucleic Acid Techniques (NAT): for detection of mycobacteria from the
speciemen, identification
of mycobacterial species and drug sensitivity.
F.
Immunological tests: Mantoux test, Interferon gamma assay
G.
Other supportive investigations: Erythrocyte Sedimentation Rate ( ESR ),
Adenosine Deaminase
(ADA) assay, Cytology, Histopathology etc.
2.
What are the clinical significance, indications and limitations of each techniques?
3.
The basics of each techniques including appropriate sampling, test principle,
test procedure and
interpretation of results.
Laboratory diagnosis of tuberculosis
Modalities for diagnosis of
tuberculosis are divided in two groups
1. Methods which provide direct evidence of presence of tuberculous bacilli in the specimen taken from the site of lesion
a. Demonstration of Acid Fast Bacilli(AFB) by microscopic examination
b. Isolation of bacteria by culture examination
c. Detection of bacterial specific nucleic acid by Nucleic Acid Technologies (NAT)
d. Detection of bacterial specific antigen
These modalities are highly specific for diagnosis of tuberculosis. But their sensitivity is low and negative results may not rule out active tuberculosis.
2. Methods which provide indirect evidence of infection by detection of immunological & other markers, indicating host’s body’s response to the tuberculous bacteria
a. Immunological tests which reflect body’s immune response if patient gets infected:
- Mantoux test
- Interferon gamma assay
These modalities indicate the infection and not the disease. So in cases of only infection with M. tuberculosis these tests may be positive even though the patient may not have developed the disease.
b. Cytology and histopathology which reflect cellular response of body against tuberculous infection
c. Erythrocyte Sedimentation Rate (ESR) & Adenosine Deaminase (ADA) test
Sample Collection:
A.
Pulmonary tuberculosis
1.
Sputum:
- Collected in disposable wide mouth container
- Early morning sputum samples collected for three consecutive days are ideal. For direct microscopy, according to RNTCP guidelines, two sputum samples are sufficient. First is spot sample & second is the early morning sample.
- If expectorated sputum is scanty, sputum samples collected over a period of 24 hours is recommended.
- For sample collection, patient should be explained properly for collection of the sputum and to minimize contamination with saliva.
- Steam inhalation or expectorants may enhance productivity of sputum.
2.
Broncho alveolar lavage (BAL)
- It is the best sample, particularly when the sputum is expectorated minimally. However it requires invasive procedure.
3.
Lung aspirate
- Trans-thoracic, CT guided aspiration directly from the site of lesion in lung would be the most informative sample; especially when sputum and BAL specimens seem to be unsatisfactory.
4.
Gastric aspiration
-Children can not collect sputum properly and usually swallow majority of expectorated sputum. This material can be recovered from stomach by gastric aspiration or lavage.
All the above specimens can be processed for Demonstration of AFB; mycobacterial culture and NAT.
B.
Extrapulmonary tuberculosis
1.
Urine
- In cases of sterile pyuria, a high suspicion of renal tuberculosis should be considered.
- Early morning urine samples collected for 3 consecutive days are ideal.
- Every day samples are centrifuged and deposits are processed further.
2.
Body fluids
- CSF in the cases of meningitis .
- Pleural fluid for diagnosis of pulmonary tuberculosis.
- Ascitic fluid for diagnosis of abdominal tuberculosis.
- Synovial fluid in cases of arthritis.
All the above samples can be processed for demonstration of Acid Fast Bacilli, culture, NAT, ADA measurement and cytological examination for evidence of tuberculous infection.
3.
Pus
- In case of cold abscess, pus can be taken aseptically & examined for demonstration of bacilli, culture examination and NAT.
4.
Lymphnode
- In case of lymphadenopathy, lymphnode biopsy or FNAC should be taken for histopathological and cytological examination. This can also be processed for demonstration of Acid Fast Bacilli, culture and NAT.
Sample processing:
A.
Preparation of samples for microscopic and culture examination.
Purpose:
- For concentration of bacilli to have higher positivity rate.
- For homogenization of sample to process further.
- For decontamination of samples, which kills all the organisms except Mycobacteria.
Methods:
Sputum / Broncho alveolar lavage / Gastric aspirate
1. Petroff's method:
In a conical bottom test tube, the specimen e.g., sputum is mixed with equal amount of 4% NaOH. The mixture is incubated at 37° C for 30 minutes. NaOH will homogenize the sputum sample and kill majority of commensals present in sputum and saliva. It is then centrifuged. After centrifugation, bacilli will be concentrated in deposits which can be used for microscopic and culture examination.
Caution: Prolonged incubation of the specimen with 4 % NaOH may also affect viability of Mycobacteria.
2. Cetyl pyradinium chloride (CPC) + NaCl
CPC is considered the best decontaminating agent. It does not affect the viability of Mycobacteria even after prolonged incubation. Particularly, when the sample is to be collected from a remote place, sputum should be collected in CPC containing container and then transported to Laboratory. The sample will be decontaminated during transit time and Mycobacteria will be preserved. The mixture of CPC with sample is then centrifuged and deposit is used for microscopic and culture examination.
3. N-acetyl L - cysteine (NALC) + NaOH
The concentration of NaOH is kept 2%, which can decontaminate samples without affecting the viability of Mycobacteria. The added NALC will act as a mucolytic agent and homogenize sample thoroughly.
Urine:
Oxalic acid is used to decontaminate urine specimen. Homogenization is not required for urine specimen. The urine collected on three consecutive days is centrifuged and deposits are incubated with oxalic acid. All the three processed deposits are mixed and neutralized. The collected material is centrifuged and deposit is processed further for microscopic and culture examination.
Microscopic Examination:
For demonstration of Acid Fast Bacilli
Methods:
1. Z N stain
a) Hot stain : Routine Z N stain involving the heating of the smear as a mordant.
b) Cold stain(Kinyoun stain) : A modified Z N stain that does not involve the heating process, but has increased concentration of phenol in carbol fuschin, increased duration of stay of the primary stain on the smear & a wetting agent; tergitol, to suffice the need of the mordant instead of heat. This method prevents alteration in morphology of the Mycobacteria.
2. Auramine-phenol ( needs fluorescent microscope)
Role of microscopic examination in diagnosis of tuberculosis in routine practice:
• Every specimen (other than blood and stool) received to evaluate the infectious aetiology , must be investigated by Z N stain examination.
• Z N stain is the easiest and quickest test
• It needs good quality samples
• Limitation of microscopy – It can diagnose < 50 % of active tuberculosis
• Sensitivity of ZN stain is 10,000-100,000 bacilli / ml
• Fluorescent microscopy can increase sensitivity by 2.5 times
Culture examination:
Significance
of culture methods:
- Sensitivity is very high, as low as 10 bacilli / ml of specimen can be detected.
- The isolated Mycobacteria can be processed further for species identification and antituberculous drug sensitivity.
Methods:
1. Solid culture media: L. J. medium
- The processed specimen is cultured on LJ medium slants.
- The bacterial growth (colonies) will appear after 20 - 40 days of incubation.
- The isolated Mycobacteria are processed further for biochemical reactions, to differentiate M. tuberculosis (MTB) from Mycobacterium other than tuberculosis (MOTT).
The following tests will be positive for MTB
1. Niacin test
2. Nitrate reduction test
3. Catalase test.
2. Liquid culture media:
Middle brook medium, Dubo's medium
3. Automated culture methods:
Processed sample is inoculated in the specified Middle brook medium. The Mycobacterial growth in the medium will release carbon dioxide. This can be identified by automated methods based on various principles.
e.g. BACTEC MGIT will detect bacterial growth and carbon dioxide released by fluoro-metric method
BacT Alert will detect bacterial growth and carbon dioxide released by colorimetric method.
Growth can be detected as early as within 11-14 days of incubation, being indicated positive by the different indicator systems.
Antibiotic sensitivity:
The commonly used method is 1 % Proportional method
Principle:
Clinically significant resistance to any anti-TB drug is defined as an in vitro growth, in the presence of the critical
concentration of the drug, that is equal to or greater than 1% of the growth in
the absence of the drug.
This can be performed by two different ways
On Solid media (Conventional method):
The Mycobacterial isolate is cultured simultaneously in
1. Control LJ medium (not containing any anti tuberculous drug).
2. L J Medium slants containing a critical concentration of individual anti-TB drug to be tested for sensitivity.
They are incubated aerobically at 37° C and observed at regular intervals till growth appears on control slant. At the same time, if test slant shows bacterial colonies more than 1% of colonies on control slant, the bacteria is interpretated as being resistant to that particular anti-TB drug which is present on the test slant.
In
Liquid medium (Automated method)
The Mycobacterial isolate is inoculated in 3 bottles
1. Bottle without anti-TB drug inoculated with bacterial suspension.
2. Bottle with anti-TB drug inoculated with bacterial suspension .
3. Bottle without anti-TB drug inoculated with 1:100 dilution of the above bacterial suspension.
If bottle no. 2 is indicated positive earlier than bottle no.3, the isolate is considered resistant to that particular drug.
Other
methods of anti-TB drug sensitivity
Resistance ratio method
Absolute concentration method
Nucleic acid technologies (NAT)
These are useful for
1.
Detection of M.TB in specimen
The bacterial specific DNA / RNA sequence can be identified in the specimen.
Technologies available are
Polymerase chain reaction,
Gene probe,
Nucleic Acid Sequence Based Assay,
Gene X-pert
DNA fingerprinting – IS 6110
Sensitivity of these methods is very high. Speciemen containing as low as 1-10 bacilli / ml can be detected as positive.
2.
Mycobacterial species identification
Method: Line Probe Assay
3.
Anti-TB sensitivity
Method: Line Probe Assay (detects resistance to first and second line AKTs),
Gene-Xpert (detects resistance to Rifampicin)
Modalities providing indirect
evidence of TB infection
1. Mantoux test
The reaction to the intradermally injected tuberculin is a classical example of
a delayed (cellular) hypersensitivity reaction.
Procedure:
A
standard dose of five tuberculin units (TU) (0.1ml) is injected intradermally
on the volar aspect of forearm (left side is recommended uniformly). The
patient is instructed to keep the test site clean, uncovered, and to not
scratch or rub the area. The Mantoux skin test should be read between 48 and 72
h after administration. The basis of reading is the presence or absence of
induration, which may be determined by inspection and by palpation. For standardization, the
diameter of induration should be measured transversely to the long axis of the
forearm and recorded in millimeters.
Interpretation:
-
Reaction of more than 15 mm in size is considered positive
-
No reaction or reaction size < 5 mm is considered negative
-
5 to 15 mm of reaction size should be interpretated by correlation with other
clinical and epidemiological parameters
2.
Interferon gamma (INF-γ) - assay - IGRA
It
is an in-vitro assay to test cell mediated hypersensitivity against tuberculin
antigen.
Procedure:
Patients’
blood is incubated with tuberculin antigen in the laboratory; If patient will
have prior exposure to TB bacteria, the sensitized T cells on exposure to
tuberculin antigen, will release INF-γ. This released INF-γ can be measured by
ELISA test.
Note:
Positive MT and IGRA tests indicate infection ; and not necessarily disease.
Histopathology
& Cytology
In
following conditions, a biopsy may be
required
1.
Lymphadenopathy: lymphnode biopsy
2.
Pulmonary lesion: When sputum or broncho-alveolar lavage don't give any
conclusion; according to site of lesion, trans thoracic or bronchoscope guided
biopsy may be taken.
On
histo-pathological examination, presence of granulomatous lesions with or
without caseation necrosis is most commonly suggestive of tuberculosis.
In
following conditions, specimen may be taken for Cytological examination
1.
Body fluids: Pleural fluid in pleural effusion, Ascitic fluid in ascitis, CSF
in meningitis, synovial fluid in arthritis etc.
- Increased WBC count in fluid
with presence of predominant lymphocytes favors diagnosis of tuberculosis
2.
Fine needle aspiration for cytology (FNAC) taken in cases of lymphadenopathy
- Presence of granulomatous
cellular infiltrate favors diagnosis of tuberculosis
Adenosine
Deaminase (ADA) assay:
- ADA is an enzyme produced by lymphocytes in the
presence of intracellular tubercle bacilli.
- In case of effusion, ADA should
be analyzed in fluid. ADA can be measured by automated
and semi-automated methods
- The cutoff value for ADA
Pleural fluid,
Abdominal fluid, Synovial fluid: 50 IU / ml
CSF: 10 IU / ml
- Increased ADA level (above
cutoff value) in fluid with higher lymphocyte count is most likely associated with
tuberculosis.
Erythrocyte
Sedimentation Rate
It
is one of the commonest supportive investigation to be carried out in each suspected
cases of tuberculosis. Though having very poor predictive value, it can help a
lot when used in combination of various other clinical, radiological and
laboratory parameters. It also provides a significant prognostic value in
patients on anti tuberculous treatment.
Exercise:
A
18 year old male patient presented with low grade fever and cough; X-ray
chest is suggestive of pulmonary tuberculosis. Previously also patient has
taken AKT for the period of 6 months; since 2 months he is off the treatment.
We need to evaluate further for proper management of patient.
Q.1 Which samples can be collected? Find the containers are
useful for collection of respiratory samples.
Q.2 Which staining methods can be used for demonstration of Acid
Fast Bacilli?
Q.3 Which media are used for culture?
Q.4 Which anti tuberculous drugs should be tested for
sensitivity?
Q.5 Enlist the Nucleic Acid Techniques for TB
Q.6 Which immunological test is used?
No comments:
Post a Comment